About Conditions Navigated.
Joyce’s Story - Alzheimer’s
My mom, Joyce, was my best friend. I often think if I had known then what I know now, my mom might have lived a better quality of life after her diagnosis of Alzheimer's. You see, my mom had a trajectory in her health that led to her dementia. I still remember her on the toilet in the bathroom, unable to evacuate. In my mind, she had warped back to three years old because she could not fully comprehend what was happening, and even with my knowledge, I did not recognize that something so simple as going to the bathroom had gone so wrong over time. She was incredibly constipated, and it haunts me to remember that she needed urgent medical intervention for a normal bodily function. She apologized when I tried to help as she was exhausted and confused from a task I had taken for granted she had remembered how to do. I told her not to worry; she had looked after me many times when I was little, and this was the least I could do. To read more, scroll below.
My Story on Complex Regional Pain Syndrome - CRPS
About five years ago, I sustained one of the worst ankle fractures called a tri-malleolar. The surgeon repaired it with 12 screws and a titanium plate. I developed CRPS post-surgically, and the pain felt from this condition was the worst I have ever felt. Trophic changes, like increased hair growth, and skin changes like redness, are highly associated with this condition. It’s important to be an advocate for yourself and see your doctor immediately if you notice these changes after an injury.
I still remember sitting in a tub, trying to calm the fiery burning associated with the condition and wishing I would die. Eventually, I trusted my knowledge as a practitioner and investigated every avenue of care for a person with CRPS. Many tools helped me manage my condition, and one essential intervention was improving my fibre intake to improve the health of the microbiome in my Colon, and choosing foods I was less reactive to in decreasing my overall inflammation. CRPS is now known to occur in those with a higher inflammatory load. By modifying my foods and trusting in the power diet had on my physiologic systems, among other lifestyle changes, I improved my resiliency and put my CRPS into remission. To read more, scroll below.
Burning pain and trophic changes are associated with CRPS and it’s important to seek medical attention immediately
CRPS & Removal of Hardware. A Decision that Requires Team Management
If we prepare adequately for something that is important to us, decide based on evidence, and use the right tools, we can navigate any storm. Confidence comes from adequate preparation and then the rest is trusting in yourself and your body to heal you. To read more, scroll below.
My story about Breast Implant Illness (BII)
When I was 17, I made one of the poorest decisions I could make. I remember staring at the pages of Brooke Shields in teenage magazines amongst other models and wishing for larger breasts. I was immature and decided I needed augmentation. I remember developing strange allergies and having long-standing fatigue from mononucleosis at university. I also fell into a bit of depression which had not matched who I was before my surgery, a happy-go-lucky teen. To read more, scroll below.
Hashimoto’s Thyroiditis
During the years I had implants, I did not have much energy. I don’t think I connected the two together until I started to have numerous symptoms appear like fatigue, sinus allergies, constipation, eye itching and watering in the evening, armpit swelling, and itching of the breast and neck post-Covid infection. Hashimoto’s Thyroiditis is an autoimmune condition that includes about 97 percent of Hypothyroid cases. My mom had this condition show up before Alzheimer’s and I had concerns because we inherit our mitochondria from our mothers and hence I did not want to follow the same pathway. My brother also has developed Hashimoto’s and I was beginning to wonder about my own metabolics with all of my symptoms.
In the Functional world, a heavy metal load is one of the stronger causes associated with the development of Hashimoto’s. Gliadin, a wheat protein, is also suspected to be involved in the progression of the development of the disease. When we have food sensitivities (IgGs), not allergies (IgEs), our body usually has not digested the food properly into single molecules allowing for proper digestion and delivery of micronutrients to the cells. When gliadin enters the bloodstream in a peptide chain versus a single amino acid, the body recognizes it as foreign and develops antibodies against it. The antibodies then go on a hunt in our immune system to try and locate similar proteins to mark them as foreign so the body can mark it for removal from the body. The tissue most similar to the gliadin protein is the thyroid gland. In simple terms, continued gliadin ingestion and poor digestive processes cause a condition where the thyroid gland is attacked and an autoimmunity condition emerges.
When I think back in my history I had a few episodes of fatigue where it was so bad I wanted to sit down on a rock to take a break from a hike. This was not the energetic able-bodied person that I was. I knew that I was still young and that this feeling was not normal for me. During Covid, I believe I contracted the virus early in its inception and the flu was unlike any other in that I was tired, really tired for a few months after most symptoms had resolved. I could not get my energy back. This became known as long Covid and I appeared to have it. To read more, scroll below.
-
My mom, Joyce, was my best friend. I often think if I had known then what I know now, my mom might have lived a better quality of life after her diagnosis of Alzheimer's. You see, my mom had a trajectory in her health that led to her dementia. I still remember her on the toilet in the bathroom, unable to evacuate. In my mind, she had warped back to three years old because she could not fully comprehend what was happening, and even with my knowledge, I did not recognize that something so simple as going to the bathroom had gone so wrong over time. She was incredibly constipated, and it haunts me to remember that she needed urgent medical intervention for a normal bodily function. She apologized when I tried to help as she was exhausted and confused from a task I had taken for granted she had remembered how to do. I told her not to worry; she had looked after me many times when I was little, and this was the least I could do.
I remember tucking her into bed and feeling uncomfortable that I couldn't help her, and was worried over what I had witnessed. The new medications had also created more confusion in an ecosystem that could not purge byproducts of digestion. It had become increasingly toxic to the point of affecting her clarity and thoughts. I asked myself how a person not functioning well could take medicine and expect it to work in a stressed biological environment. I thought the best treatment would have been to have focused on her constipation, at the very least, for her memory and detoxification. Often, I think back to that day and wish that I had taken her to the hospital because what she was experiencing was an emergency.
Joyce was the most fantastic soul that had helped and held the hand of many patients. She had always worried about developing dementia as the medical model and diagnostic labeling had taken the beauty of many individuals down to a label that was supposed to now describe who she had become. She feared the label and the destruction of the mind. I later could understand this fear in a comment she made in a moment of clarity, "I don't want to leave you, Lisa." Eventually, her mind and body did leave me, and I was left without a mother, my son a grandmother, my dad a spouse, my extended family a sister, and her patients a loving caregiver.
From the Functional model, I now know that her condition was a product of many root causes. If I had addressed some of her root causes, she might have recovered early on or had a slower progression in the disease process. As a younger person, had she become aware of her body's sensitivities, she might not have developed Alzheimer's. She suffered from early allergies, asthma, eczema, psoriasis, poor sleep, poor water drinking, constipation, lack of exercise, fluctuating hormones, hysterectomy, dyspepsia, H. Pylori, Hashimoto Thyroiditis, depression, hair loss, cold intolerance, severe seafood intolerance, brain fog and ultimately dementia. How could all these be treated in isolation? No root cause was investigated but each symptom was viewed singularly and medicated.
Joyce is gone, but her story has catapulted me into helping many and speaking out. If I can get just a few people to think about their diet and lifestyle decisions more in their overall health trajectory, I have made a small difference in this world. I often ask myself what led to her illness, and I can tell you precisely what her triggers were and the mediators that could have made her better. She had inflammation from digestive issues, and every branch pointed to that. How had someone missed this? There was no system to connect the dots. She was treated as Joyce with Alzheimer's in a system that she worked in, loved, and feared. Joyce was a beautiful woman with love who failed to see the connections in her choices in life that later took her down system-by-system. Every little choice we make daily matters to our overall health and can decrease our allostatic load giving us more resiliency.
The Weeds in a neurodegenerative disease
I remember everyone in my family in distress over how to help my mom, including my dad, who is still a practicing GP. I remember him saying he felt frustrated that he couldn't help her. There was no medication to cure her, and we had exhausted all medical tests available at that time. I would rewrite this story by hugging him and saying, "Hey Dad, there is something we could do..." I would have modified her diet as her best intervention. I would have changed many of her lifestyle habits to include more water drinking, exercise to increase bowel tone, playing to decrease stress, and focusing on her sleep. Our family has had longstanding issues with dietary sensitivities; looking back, the answers to her digestive sensitivities were staring at me. Now I have the training to identify this, and I promise my mom to help as many as I can.
-
My Story on Complex Regional Pain Syndrome (CRPS) - Fear of the unknown of the "Complex" and the alternative medical label "Suicide Disease"
About five years ago, I sustained one of the worst ankle fractures called a tri-malleolar. The surgeon repaired it with 12 screws and a titanium plate. I developed CRPS post-surgically, and the pain felt from this condition was the worst I have ever felt. Trophic changes, like increased hair growth, and skin changes like redness, are highly associated with this condition. It’s important to be an advocate for yourself and see your doctor immediately if you notice these changes after an injury.
I still remember sitting in a tub, trying to calm the fiery burning associated with the condition and wishing I would die. Eventually, I trusted my knowledge as a practitioner and investigated every avenue of care for a person with CRPS. Many tools helped me manage my condition, and one essential intervention was improving my fibre intake to improve the health of the microbiome in my Colon, and choosing foods I was less reactive to in decreasing my overall inflammation. CRPS is now known to occur in those with a higher inflammatory load. By modifying my foods and trusting in the power diet had on my physiologic systems, among other lifestyle changes, I improved my resiliency and put my CRPS into remission.
I have been a healthcare practitioner for 20 years and have seen many patients with varying degrees of soft tissue complaints. More often than not, I noticed a pattern that I could not ignore. Many had symptomatic complaints that have their roots in the digestive system. Patients would often get better with my rehab work, but they would sometimes return, especially after holidays or travel, where they changed their diet and would experience a strange flare affecting their nervous system, muscles, and joints. If I could help patients understand the physiologic effects of better food and lifestyle choices, their quality of life and overall resiliency would improve.
-
I have often been called the connector to help my own patients navigate the steps they need to take to support their health. When I decided to remove the hardware from my ankle fracture that was beginning to affect my life after five years of it taking up residence in my body, I became my own coach and set myself up for success. I believe in the Functional Model and it gave me the confidence to make the important decision in removing my titanium plate, 10 solid titanium screws, and two hollow long titanium screws.
I also know from being in healthcare that we often get stuck in the weeds of our condition(s). We need to take back control and accept that our health is our responsibility; not someone else’s. We also need to understand that fear in a condition comes from navigating an unfamiliar pathway.
Important decisions take adequate reflection and preparation, and then what follows is trusting you’ve done everything you can for things to work out in your favor. Top that with a little neurolinguistic brain programming (NLP) by repeating your favorite mantra like “You’ve got this,” and you have a direct link to the immense power of the subconscious mind.
The Functional model looks for the root cause(s) for a condition. CRPS is no longer known as the brain blip that happens out of our control but has inflammatory roots. For me, my allostatic inflammatory load was high having had breast implants since the age of 17 along with the stress of five years of my physical and mental body dealing with CRPS and the titanium hardware from my tri-malleolar ankle fracture. Functionally, if I took a step back and looked at the lens of my situation and removed elements in my life’s allostatic load bucket, my health should get better.
In the past 18 months, I noticed strange occurrences that were not present before my fracture. The hardware appeared to be causing some odd symptoms. When I would rollerblade, which was a love of mine from having figure skated for 12 years, I would flare afterwards by developing an ache on the side of my lower leg and some mild burning in my foot. These symptoms were getting worse with exercise that challenged my fibular bone and the plate in an intricate game of tug of war. The side of my leg felt stiff and immobile. Also odd was that if I were to develop a cold or have some sort of immune system stress, the inside of my ankle would itch where my hardware went into the medulla of the bone. I remember reading in research on CRPS that around 13-18 percent of patients would have remission when these types of screws were removed. That was a pretty good statistic.
Even an Epsom salt bath would leave me feeling as if my right leg was stinging in the area of the hardware. I felt like I was literally rusting. One of my friends is a chemical engineer and said it sounded as if my soft tissue was reacting to the titanium. Also in the research, it is not common to have reactions to this type of metal though it is my belief that our body does not react to titanium well over time as more loads are placed on our body, and our body engages an inflammatory process to heal the body. It’s a natural occurrence but wrong. Perhaps metal hardware is considered a big wood splinter. It is certainly logical to assume this because it is not our own soft tissue; it’s foreign.
The Surgery
After enough confidence in knowing my body and having put my CRPS into “mostly” remission, I decided it was time to remove the hardware. I felt ready inside and out. I have had two doctors for my health since I developed CRPS, with one being my GP and the other a Functional Medicine Doctor who has been with me from the start listening to my story and helping to refer me to support my needs. With this support, I ended up with two referred consultations with Orthopaedic Surgeons.
The First Consult - Know When to Say, “No”
I had booked to see a Surgeon from a popular Rehab Centre in Victoria, BC, one that many athletes consulted. I also took my son because of his interest in becoming a surgeon. I brought a protocol for surgery for CRPS patients that explains that CRPS is inflammatory and General Anaesthetics should not be used, and to use blocks. It also listed medications to use prior to any surgery to offset inflammation and specific components for the Anaesthesiologist to use during the surgery to make the outcome a success, i.e. not to flare the CRPS beast.
During my discussion with the surgeon, I mentioned my desire to remove the hardware and my recent onset of increasing symptoms to my hardware. His response after hearing I had CRPS was it was likely arthritis and suggested that he would not do the surgery if he was me. He also gave me my document back that contained the proper blocking procedure for a CRPS patient. My son also noticed with his spidey senses that the surgeon kept looking at his watch. I had a strong feeling he resented the information that I had brought and that he was not confident in operating on me. I literally had to dredge this information out of him.
I told the surgeon that I had been a figure skater in the past and that the discomfort was not in the joint but at the side of my leg after blading. I also mentioned the itching over my medullar screws (screws into the inside of the bone) which he ignored. He continued to deny that “I” was feeling stiffness from the plate. I then reframed his comment with a question, “Okay, but what do you think the hardness of titanium is to bone?” He quickly responded - “same”. Many of you may have a teenager that Googles and my son is no exception to the virtual encyclopedia. My son stared at me and he’s very good at chemistry. He knew the surgeon’s answer was not correct. After the appointment, my son quoted Google and said, “Titanium alloy is five times stronger. Calcium is considered a light metal having a density of 1.55 g/cm3. The density of titanium is 4.506 g/cm3. Titanium is heaving and less elastic than bone.” So when I was saying to the surgeon that I felt a stiff pull from the titanium this is what I was referring to. I felt unheard and frustrated.
I knew I had reached an endpoint with the surgeon and that he was not the right one for me. I said to the surgeon that my dad who is also a GP said that it would be tough to find a surgeon that would want to operate on me having CRPS. I was about to say it would take a special person who attempted to hear and understand my concerns, but he immediately responded and said, yes, “I would not do it if I were you, but if you really want me to I will”. He also told me that I might be left disabled as my condition may likely get worse with further surgery. To this, I said thanks and we left.
Consult 2 - Someone who listened
After a few months of grounding after the first consult, I visited a surgeon in Nanaimo who was a foot and ankle specialist. I had heard good things about her and was aware of several of my own patients who had good results with her skills and care.
During the first five minutes of the appointment, I could tell I had my surgeon. I also took my son and his big reframe comment was that I was heard. The surgeon said that she would respect the tissue. In response to the blocking protocol I had with me, she arranged for a pre-consult with an anesthesiologist. She ended the appointment by asking me if I had any questions and my big one was, “Are you comfortable doing my surgery”? Her answer was yes.
The Anaesthesiogy Consult
This consult was the most important to set the framework for the operation. After discussing and handing the blocking protocol to the Anaesthetist, he smiled and discussed a bit about my field, Functional Nutrition, and the education of a general anesthetic. He asked me the biggest question for a CRPS surgery on whether I wanted a General or a Spinal. He said being an older doctor he would opt for a Spinal—he said they are easier on the body. The literature I reviewed suggested that a General could make a CRPS patient flare. The key really in the surgery is to prevent afferent signals to the brain by blocking individual nerves. The longer the better. I had a lovely meeting filled with mutual respect and time was taken by the medical professional to be empathetic.
A Spinal or Regional block was my choice. I had also been offered to bring a headset to listen to since I would be awake for the procedure. It would likely block the acoustic sensory. This notation was made in my chart for the Operating Room attendees.
Pre-Preparation for Surgery
With the date fast approaching, I prepared mentally for the surgery by listening to Hypnosis Downloads surgical preparation and Fast Natural healing tracks (see links provided on this website). I also arranged for compounded glutathione to inhale to help decrease any current inflammation so my body could handle the surgery with ease. Glutathione is one of the most potent antioxidants and is considered in the Functional world a master antioxidant. N-acetyl-cysteine or NAC as is often referred to, is a precursor to glutathione and in the Dutch Guidelines on CRPS is used orally with alpha lipoic acid as an antioxidant. I wanted to make sure my body was ready with antioxidant armor. My compounder had highly recommended using two weeks prior to my surgery and two weeks after for optimal healing. It would also boost the methylation processes in my liver again for successful healing.
I also had my Oska device to use for post-surgical pain and inflammation (see the link on the website and use the “Loki” code for a $55 USD discount. Any affiliate amounts will be donated to my favorite animal rescue charities.). Oska is a device that is used to help heal mitochondria and it worked for me to decrease my CRPS symptoms. I knew it would be a great ally for post-surgical swelling, redness, or burning pain. Having tools makes you relax more and remember it’s never one thing but a full toolbox that helps alleviate fear you have for any chronic condition. I also had crutches, an ankle cryo-cuff, and a water tank for cold circulating water post-surgery. For rehabilitation, I set up physio appointments for support and a few counseling appointments to ensure I had my support team.
Meeting the Anaesthesiologist.
While I was awaiting surgery, I took my headset and hypnosis tracks to continue to listen to for motivation prior to the surgery. I was then wheeled into a hallway where I met my surgeon and the anesthesiologist prior to entering the surgical room. Dr. Capstick, a Staff anesthesiologist, told me he was one of the few anesthesiologists that knew how to do blocks and that he was also familiar with CRPS. I was lucky and he also was amenable to discussing the cocktail for my surgery from the notes made from my pre-surgical consult with my original anesthetist. We discussed lidocaine blocks and he suggested using bupivacaine because it would provide 17 hours of a block versus 1 hour for lidocaine. This really should be a formalized protocol offered for CRPS patients. In addition, he used IV clonidine and a “compromised” 10 mg of ketamine vs. 30 mg that I had suggested. Ketamine had given me a rather uncomfortable ‘travelling through the speed of light’ sensation before during another surgery and he did not want me to suffer the same. During that surgery, I was under a general for a trunkal surgery and I literally thought I had died and had immense love for my family. It was scary and strange at the same time.
We needed Ketamine to block the NMDA receptors to eliminate or reduce any post-surgical flares of pain. Keep in mind that this was a new protocol we were using but I felt very content with his knowledge. I trusted him.
The Jazz Party in the Operating Room
I had my headset ready to block the sounds of the drill during surgery and I felt very relaxed. I was not worried and continued to hear the positive reinforcement from my hypnosis tracks before my surgery. I kept telling myself that this was a healing surgery. I did not let my mind go to the negative. The nursing staff offered to pipe my jazz music into the room during the surgery so everyone could hear it. It was soft jazz and we all enjoyed it helping to turn a serious surgery into a more relaxed event. I was also offered to view the screen to see the blocks used on my leg. The surgeon blocked the popliteal and sciatic nerve and the effects took about 15 minutes to set in. My leg felt warm and heavy. The surgeon also used numerous injections of lidocaine as well during the surgery for mini blocks. I was offered something for relaxation prior to the injected local blocks but I turned it down — I know, right? I was in the zone.
I heard a little bit of drilling during the surgery and remember my mouth feeling very dry but both did not bother me. Being awake during a surgery might seem scary to many but it was an easy procedure with no anesthetic after-effects - no nausea and no gas.
During the procedure, one of the longer screws on my inner ankle had broken trying to remove it and because I was awake the surgeon was able to ask for consent to get it out. I told her to go for it since I did not want to worry about my body flaring because of a piece of metal left in my bone.
I was not in the recovery room long because my vitals were excellent and my only sequelae from the surgery was a painful posterior calf muscle for a few days. The Anesthesiologist told me it was likely due to the tourniquet being tight to prevent bleeding when they had to drill into the bone to remove the broken screw. The discomfort did go away but it is important to mention to your surgical team to use caution in surgical tourniquets to prevent CRPS flares post surgically. The pressure might have irritated a more-sensitive individual depending on the case.
The Initial Week Post Surgically
I know many of you are likely wondering if the thought of CRPS returning was in my head. I would have to say of course it was but I kept it at bay and had prepared prior to the surgery for a positive outcome.
I utilized a few key nutraceuticals for pain post-surgically. They included PEA, Curcumin, Vitamin C (started two weeks prior to surgery as well), vitamin D (4,000 IU), Boswellia serrata (2 capsules per day), and my topicals (3) - magnesium/carnosine blend (Lactigo), compounded DMSO (50% gel) and a compounded Ketamine blend consisting of Amytryptilline, Clonidine and Lidocaine (7%). I used these on my spine to target the leg in case I needed it for muscle spasms or discomfort. A local compounder was key to my overall success. As a Functional Nutritionist, I knew that even Advil, Naprosyn, Celebrex, or Aleve could affect my gut microbiome like antibiotics so I wanted to use other means to help my body overcome a stressful physical and mental event. I remember only using a total of three Celecoxib and Tylenol for pain. One Celebrex and 1000 mg of Tylenol pre-surgically, and one of each post-surgically in the days following. That’s all I needed.
Probiotics and prebiotics were key as well because during orthopaedic surgeries antibiotics are given through IV to prevent infection. This will disrupt the microbiome.
The Zone
I don’t know if many know about ‘the zone’ that occurs in a positive growth mindset but I have achieved this a few times. This surgery was one of them. I managed my thoughts well, letting more positive than negative enter. The whole surgical process flowed.
If I needed reinforcement, my spouse was there to remind me how I’ve gotten through many obstacles before along with utilizing hypnosis downloads to coach my conscious and subconscious. I knew I had prepared for my surgery and I felt confident with my team. I also felt that an empathetic bridge existed between me and my surgeon, the anesthesiologist, and the attending nurses. All I can remember about the day was everything going right down to obtaining the 1 out of 12 Anesthetists that knew how to do blocks. A positive mindset was key to unlocking my successful surgery.
The Functional Prep
I respected my gut microbiome with healthy food pre and post-surgically using topicals versus oral medications so that my liver had the least effect from the drugs. This would help bolster me in a faster recovery the less my liver had to methylate (clear toxins). The surgical block was also key because I did not have to recover from a General Anesthetic. Healthy whole foods, sleep, meditation, nutraceuticals/topicals, the team I chose, and the support from my family including my husky dog Loki all worked wonders in my recovery. I feel great. I now rollerblade with ease and comfort on my natural leg - no more hardware!
Thank you to Dr. Jim Capstick (Anaesthesiologist Nanaimo Regional Health) and Dr. Jane Yeoh (Foot and Ankle Orthopaedic Surgeon) for your compassion and knowledge. Working together helps to make for a successful surgery and I am thankful for their support and care.
-
When I was 17, I made one of the poorest decisions I could make. I remember staring at the pages of Brooke Shields in teenage magazines amongst other models and wishing for larger breasts. I was immature and decided I needed augmentation. I remember developing strange allergies and having long-standing fatigue from mononucleosis at university. I also fell into a bit of depression which had not matched who I was before my surgery, a happy-go-lucky teen.
At age 26, one breast felt strange and had ruptured. I had to have surgery to remove the silicone implants and was informed that there was a much safer version available called saline which if ruptured would cause no harm. The surgeon had said the silicone from one implant had literally collapsed in her hands during the replacement augmentation. At this time, I clearly remember having more sensitivity to cold and would have to have regular baths at night to get warm. My metabolics appeared to be affected even though I was such an active outdoor enthusiast.
In my early forties, one of the implants from the previous surgery had ruptured and I was told that I could leave it in without any harm to my body. At this point, after having a child, I decided further surgery was not for me and left them both in because the implants were small and under the pectoral muscles hence not too noticeable. Over time, my allergies increased to develop puffiness and redness in my eyes and my sinuses continually drained at night. I also eventually developed an itch so severe in one of my breasts that I decided at age 52 to have an explant because too many symptoms were affecting the quality of my life. The surgery went well and my allergies improved and with each passing year, I feel better. Healing takes time.
Prior to the surgery I had joined the breast implant illness group (BII) on Facebook to find out more information on explant surgeons. Unfortunately, the best explant surgeon was difficult to see because Covid had shut all flights down to the US. The surgeon I chose in Vancouver performed augmentation and explants. This was an ethical dilemma. You either help your patient to get better by believing in their story and explanting or you do the surgery because you dismiss the root cause of their symptoms and continue to do augmentation on other patients knowing that implants have a lifespan and potential associated implant illness symptoms. In my case, a heavy metal load from the implants was likely in my roots causing an early elevation of my thyroid antibodies. Heavy metal loads are often according to Dr. Isabella Wentz, PharmMD, a large metal load is often responsible for causing Hypothyroidism. Everything we do in life matters and it is all connected. The breast is not in isolation from the thyroid or other body systems. All of our components are designed to work in harmony together.
From this knowledge, I have also helped many prior to explant and after to heal from the procedure. Whole food matters in this case to decrease the Allostatic load that implants place on one’s body. Learning about detoxification and helping to decrease overall inflammation is key to a successful recovery post-explant.
I have met some who refuse to acknowledge the connection between their implants and their symptoms but every system is connected and when heavy metals and silicone leech into the capsules formed by the body’s own tissue, they can escape during explant when the capsule is not removed in its entirety with the implant into the body and it is impossible to get it out according to Dr. Chun, a world-renowned en bloc surgeon. In addition, the inflammatory contents can reside in the capsular tissue itself causing xanthomatous inflammation. This happened in my case as seen in my pathology and it caused my body to have an immune response no different from a foreign object but definitely more serious with more severe consequences. It was like having two very large splinters covered in toxic compounds.
The best advice I can give is to love and respect your body. I love my breasts now and perhaps this wisdom comes with age and from feeling unwell, but if I can prevent this from happening to others it is worth telling my story. Remember that you need a surgeon who has lots of expertise performing full en-bloc total capsulectomy surgery which aims to remove the breast implant and the entire capsule of scar tissue that surrounds it. I remember reading material from a few pathologists that if the capsule is not removed fully, the body will still have an immune response.
-
In addition to the fatigue from Covid, I also had elevated ALT, a liver enzyme. I had not had any bloodwork in the past to be abnormal particularly an organ as important as the liver which is responsible for our body’s methylation process or in other words the processing and packaging of our nutrients and purging our system of the byproducts of cellular metabolism.
The liver is important physiologically to process and package the necessary nutrients for our body’s cells and to break down drugs into forms that are easier to use for the rest of the body or that are non-toxic. It’s an important job and with an elevated enzyme, the information was telling that an issue was brewing. Physiologically, an elevated ALT is also associated with pancreatic function so I had some clues about my digestive function. Could this also create fatigue? Yes, you bet.
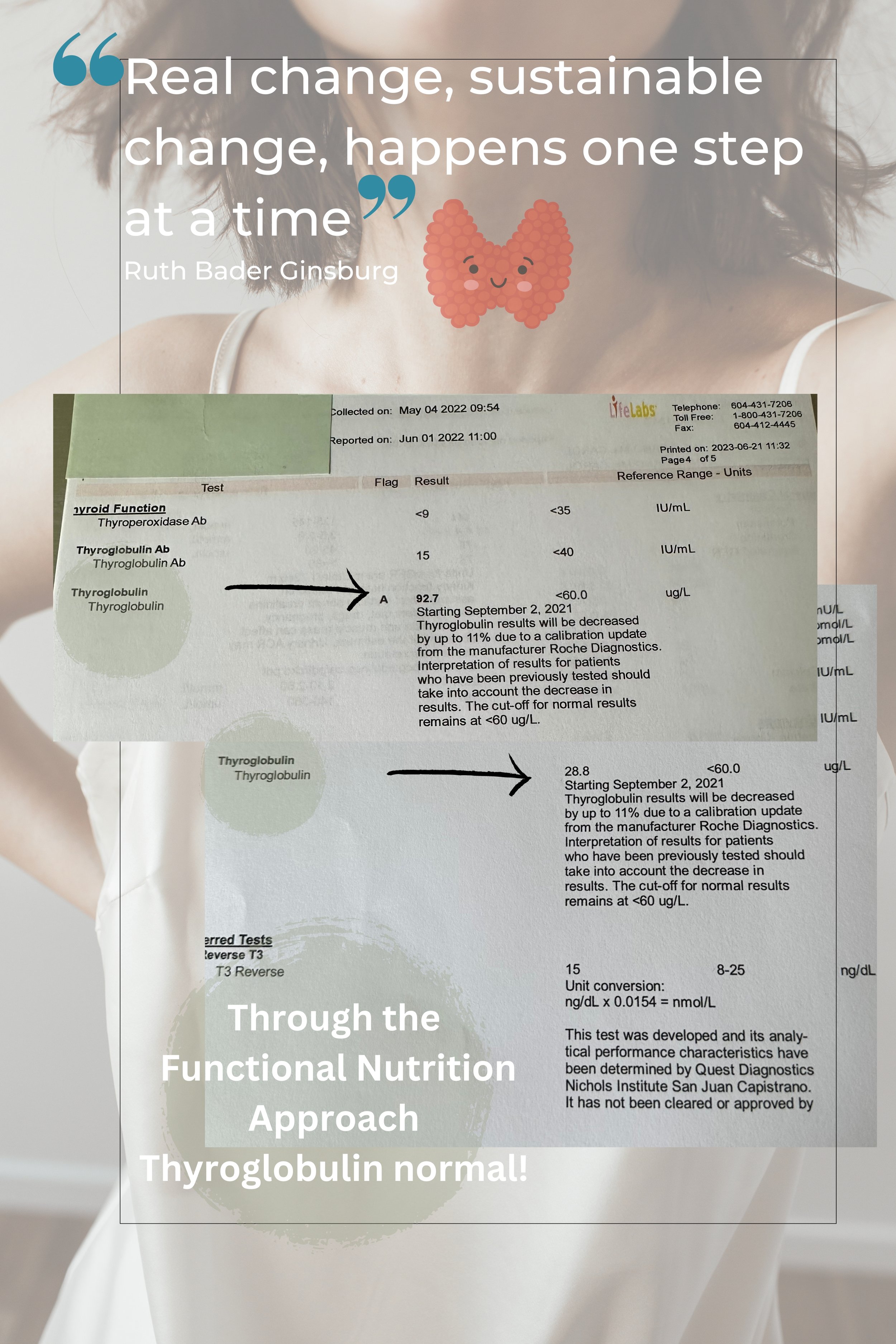
I decided to ask my doctor for a full work-up on my thyroid stating that I would pay for the full thyroid panel and not to cancel free T3 or free T4 if the TSH was normal. In many Hashimoto’s cases, TSH can be completely normal and it is important to check the full thyroid panel if suspicious symptoms arise including checking the antibodies Thyroid peroxidase (TPO) and thyroglobulin (protein). From the panel, my thyroglobulin was elevated and this can happen 10 years prior to the appearance of Hypothyroidism. In lieu of this elevation, I asked my GP for an ultrasound of my thyroid. I also was found to have nodules. This can be common at certain ages but the complete truth is that nodules tend to form more commonly alongside elevated thyroglobulin.
Typically in the current system, no pre-warnings like the above are often sounded before the process has advanced. Many are left without a full panel and only tested for TSH. When TSH is high, the thyroid has already been under attack for a long time and a greater metabolic symptomatic profile is evident. Many patients are placed on Synthroid which is mainly T4, but most with Hashimoto’s have trouble converting T4 to T3 and by taking the medication we are only patching the true problem that the thyroid gland is under attack. A Functional Nutrition Counselor is a great person to help one navigate the storm to change lifestyle habits and diet to prevent further thyroid attacks and allow healing to take place.
Our energy and vitality is a big part of our life and we don’t have to suffer but we do need to change our mindset that food matters in our health quest. Many are in denial that the fuel for our body could be a culprit but think of it this way if you have a car that uses high test fuel, would you fill the tank with regular and expect the engine to run smooth? It’s time to change from a fixed mindset to a flexible one and allow your body to flourish.
My thyroglobulin is now normal and I have amended my diet to heal the best way for me and my family has benefitted too. We are all doing well. I no longer feel the discomfort in my neck or the fatigue that I once had. We have to look for the Root cause of our issues to find out the Why not the What. I look forward to helping you navigate your storm so clear skies can shine through.